The past year has been an exciting progression of Muskoka Algonquin Healthcare’s capital redevelopment planning to replace our aging hospital sites in Bracebridge and Huntsville with two new hospitals in the future.
Just last week
we announced the future location where we plan to
build a new hospital in Bracebridge.
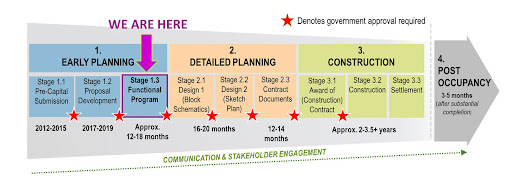
Also in December, we were encouraged by Infrastructure Ontario’s December 2023 Market Update that indicates our redevelopment
project could officially start with contract execution in 2029.
We are fortunate
to have the financial commitment of our local communities, the Ministry
of Health and our Hospital Foundations to build the best future for health care
for everyone we serve. These milestones are all great news to demonstrate our
project is on track!
Planning the programs
and services for our new hospitals in the future has been an iterative process over
the past several months. It has given us opportunity to consider changes in the
healthcare environment, advances in technology, and how we could continue to
transform Muskoka Algonquin Healthcare that will ensure a sustainable healthcare
system for decades to come. One that will position us to expand services to our
communities and solve current challenges, some recently amplified by the
pandemic such as ongoing staff shortages that contribute to frequent service
disruptions.
More than 250
subject matter experts (staff, credentialed staff, volunteers, patient
experience partners, hospital leaders and key healthcare partners) have
gathered together as User Groups to explore different service delivery models.
They have been working to define the future scope of programs and services and projected
future volumes, and identify opportunities to leverage technology and improve their
workflow while also looking at how we can close existing gaps in service.
As we worked
through our planning process, it became clear this past fall with preliminary
costing of new hospitals that replicating the existing status quo model is not
viable. With drastic cost inflation that has driven healthcare building costs
up nearly 50% in just the last year, it’s crucial that we develop an affordable
future, not only in what we build but also in how we operate services to end repeated
annual budget deficits.
Muskoka
Algonquin Healthcare is committed to a creative solution for the future that
looks forward instead of back with new hospitals that are built green and are
flexible in design. Where our two sites are complementary to each other rather
than identical, both providing 24/7 Emergency Department care, and inpatient
beds tailored to how we will provide care in the future.
Together, we
are investing in and building Made-in-Muskoka Healthcare and through innovation
and partnerships we will expand the healthcare services we can provide both within
and beyond our walls to bring care closer to home in outlying areas of the
region.
User Groups are
still working through the final pieces of a Made-in-Muskoka Healthcare solution
to meet the needs of Muskoka and area decades from now and ensure our hospitals
survive and thrive. As that
work wraps up, I am looking forward to sharing the details later this month of
how we will deliver Made-in-Muskoka Healthcare to all our communities;
healthcare that is focused on excellence, quality care and long-term
sustainability for the next 40 and 50 years.










.jpg)




